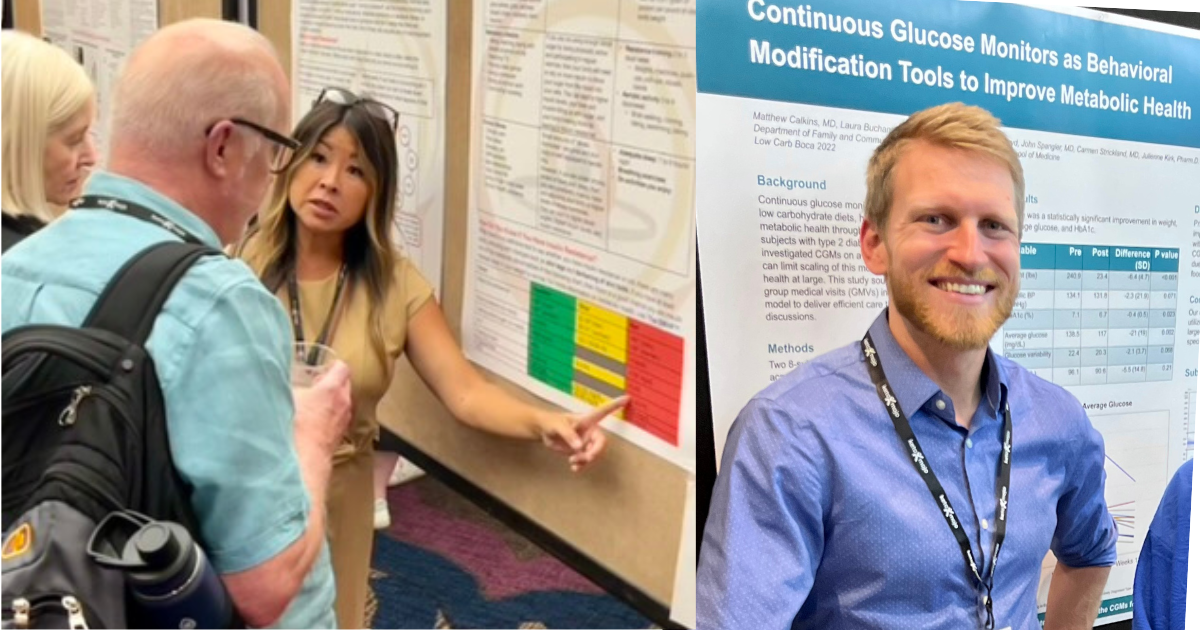
As healthcare professionals focused on metabolic health, it is a continuing goal of the Society for Metabolic Practitioners to provide the best resources and solutions to both clinicians and patients. Two new documents related to the benefits of continuous glucose monitors (CGM) merit your attention. These resources are created as part of an ongoing effort of the Advocacy Committee led by Chairwoman Jodi Nishida PharmD, MHP and Resources Committee lead Matt Calkins MD.
The first document is titled: “Why Your Patients Should Wear a CGM“, and is available for download on our Resources page. This educational and easy-to-use handout provides practical information for practitioners.
There is also a related handout titled Why You Need to be Using a CGM that can be shared with patients.
Information for Practitioners
Highlights from the “Why Your Patients Should Wear a CGM” handout include the following:
Target Population: Who Can Benefit?
One of the primary concerns that practitioners have is identifying the specific populations that could benefit from a CGM. The handout highlights that while CGMs are often associated with type 1 diabetes management, their application isn’t confined to this group. Patients with pre-diabetes, patients diagnosed with T1DM or T2DM, those looking for feedback on glucose response to nutrition, and those changing exercise routines can all benefit from using a CGM. Due to immediate glycemic feedback, CGMs can show which foods cause glucose spikes and baseline elevations that would eventually raise HbA1c. This can include people with prediabetes, hypertriglyceridemia, HTN, obesity, NAFLD or insulin resistance.
Efficacy Backed by Research
The guide includes links to studies where subjects with T2DM were given CGMs and instructed to minimize glycemic excursions based on the CGM readings. A patient-driven algorithm was employed to reduce the intake of foods that caused these excursions. Remarkably, the outcomes were found to be equal to or better than the effects seen from medications designed to control blood glucose levels.
Empowering Patients
CGMs empower patients to take control of their metabolic health by providing real-time feedback on their blood sugar levels. The handout mentions a study that demonstrated the effectiveness of CGMs in helping patients understand their glycemic response to foods without the need to count carbohydrates. With CGMs, patients can scan their sensors as often as they’d like, usually every 5-15 minutes after consuming food, to examine its effects on their glycemia.
More Than Just Food
While dietary habits are a significant contributor to fluctuating blood glucose levels, they’re not the only factor. The handout also covers additional elements that can affect blood glucose levels, including exercise, stress, sleep quality, and certain medications.
How Clinicians Can Use CGMs
One of the excellent features of CGMs is their compatibility with online portals. Clinicians can download comprehensive reports to discuss with their patients during clinic visits, thus providing a more tailored approach to managing metabolic health.
In summary, the Why Your Patients Should Wear a CGM handout is an invaluable resource that offers a nuanced understanding of the potential of CGM technology in metabolic healthcare. If you haven’t downloaded it yet, we highly recommend you do so and share this essential guide with your colleagues.
Information for Patients
For individuals concerned about metabolic health, the second handout titled “Why You Should Use a CGM” is a must-read. This patient-focused guide offers practical insights into why using a Continuous Glucose Monitor (CGM) can be a life-changing decision. Below are the key takeaways from the handout, neatly organized under thematic headings for your convenience.
Why Use a CGM?
- Family History: If you have a family history of metabolic illnesses like type 2 diabetes, a CGM allows you to proactively manage your long-term health.
- Comfort and Ease: CGMs are a painless alternative to the daily needle pricks traditionally associated with monitoring blood sugar levels.
- Immediate Feedback: Gain real-time insights into how your diet and lifestyle choices are affecting your blood sugar levels.
- Improved Doctor Visits: By sharing your CGM data with your healthcare provider, you can optimize your medication and treatment plans.
- Informed Food Choices: A CGM helps you discover which foods are causing your blood sugar levels to spike, allowing you to make better dietary choices.
- Safety: Unlike traditional finger sticks that offer a single point-in-time reading, CGMs provide a graph that shows trends over time, enhancing your ability to detect and prevent low blood sugar levels.
Factors Other than Food that Affect Blood Glucose Levels
Understanding what influences your blood glucose is crucial. The handout covers several factors beyond just food, including alcohol intake, exercise, stress, pain, medications, showers/sauna, lack of sleep, viral infections, and sleeping directly on the sensor.
Reactive Hypoglycemia
The handout also touches upon the concept of reactive hypoglycemia, a condition where your blood sugar drops too low after eating a large carbohydrate meal, leading to symptoms like fatigue, anxiety, and tremors. A CGM can help you identify how different foods and meals affect not just your blood glucose but also how you feel.
Download and Help Spread the Word
We encourage patients and practitioners to download these documents and share with others who could benefit from this information. This information could also be printed and made into a poster that could be displayed on a wall in your office.
To access the handouts described here, and to see the many other resource handouts that have been developed for you, visit the Practitioners Resources page or the Patients Resources page on The Society of Metabolic Practitioners website.